Jaundice is a common medical condition affecting newborns and in most cases goes away on its own or with mild treatment. Jaundice occurs in about 50 percent to 60 percent of full-term babies and 80 percent of those born prematurely. Babies born before 28 weeks of pregnancy are at higher risk for jaundice and need extra care.
Jaundice is caused by excess levels of bilirubin, which is a yellow pigment produced when old red blood cells break down. During pregnancy, the mother’s liver removes bilirubin for the baby, but after birth the baby’s liver must remove the bilirubin. Normally, bilirubin passes through the liver and is excreted as bile through the intestines. In some babies, the liver might not be developed enough to efficiently get rid of bilirubin and it can build up in the blood. This makes the skin and whites of their eyes look yellow.
Jaundice in newborns usually starts after the first day of life and can last anywhere from a few days to a couple of weeks. Most jaundice is not harmful to the baby and disappears when the baby’s body learns to deal with bilirubin. In some babies, the jaundice lasts longer or a baby has very high levels of bilirubin and might require close monitoring and treatment in a Neonatal Intensive Care Unit (NICU).
If jaundice isn’t treated appropriately, it can cause a rare condition called Kernicterus, which is a type of brain damage that can result from high levels of bilirubin in a baby’s blood. It can cause hearing loss, intellectual disabilities and problems with vision and teeth. Early detection and management of jaundice can prevent Kernicterus.
Types of jaundice
There are several types of newborn jaundice. The following are the most common:
- Physiological jaundice— This type of jaundice affects 50 to 60 percent of full-term newborns in their first week, typically three to five days after birth. It occurs when a baby’s liver can’t sufficiently process bilirubin. Typically this condition disappears within one to two weeks. Because their livers are less mature, premature babies are more likely to have this form of jaundice.
- Blood group incompatibility jaundice — When a mother’s blood type differs from the baby’s, her body produces antibodies that attack the baby’s red blood cells. As a result, bilirubin builds up in the baby’s blood. This condition can be prevented by treating the mother with a drug that will prevent her from producing the antibodies that will destroy the baby’s blood.
- Breast milk jaundice — A very small number of breastfed babies, about one to two percent, develop jaundice because of substances in their mother’s breast milk.
Signs and Symptoms
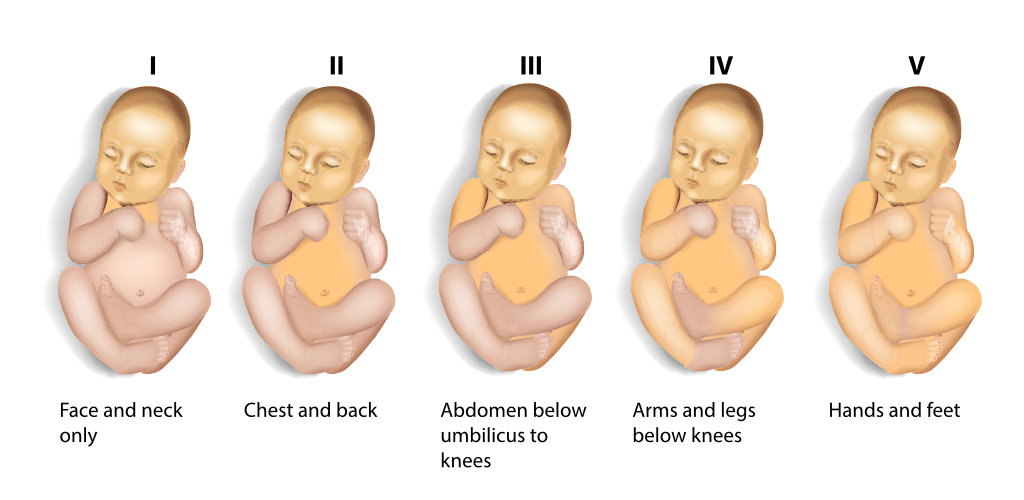
Jaundice usually appears two to three days after birth, first on the face and then as bilirubin levels get higher moves to the chest, stomach and limbs. The whites of the eyes can also look yellow. Jaundice can be harder to see in babies with darker skin color and in premature infants because of low blood flow and high bilirubin levels.
The baby’s doctor can test how much bilirubin is in the baby’s blood using a light meter placed on the baby’s forehead. This results in a transcutaneous bilirubin (TcB) level. If it is high, a blood test can confirm total serum bilirubin (TSB) level. If the level is high, based upon the baby’s age in hours and other risk factors, treatment will be necessary.
Jaundice can be more serious for babies:
- born preterm (before 37 weeks)
- who weigh less than 2500 grams (5.5 lbs) at birth,
- whose blood group is incompatible with their mothers’ blood group,
- who develop jaundice early in life, especially during the first 24 hours,
- whose jaundice has moved to the arms and legs,
- whose siblings had jaundice at birth and needed treatment
Because jaundice can develop in a baby after discharge from the hospital, parents should check their baby’s skin tone for a yellowish tint in natural or fluorescent lighting. A simple test for jaundice is to press your fingertip to the baby’s nose or forehead. If the pressed skin has a yellowish tint, then the baby may have jaundice.
See a doctor immediately, if the baby:
- Is very yellow or orange (skin color change starts from the head and spreads to the toes).
- Is hard to wake up or will not sleep at all.
- Is feeding poorly i.e refuses breastfeeding or bottle feeding
- has lost a lot of weight (more than 10% of her weight at birth),
- Is very cranky / fussy.
- Does not have enough wet or dirty diapers (at least 4-6 thoroughly wet diapers in 24 hours and 3 to 4 stools per day by the fourth day).
Treatment
Most of the time, mild or moderate forms of jaundice goes away on its own without specific treatment after five to seven days, as the baby’s liver becomes more mature.
Sometimes, babies will need help to get their bilirubin levels down. One way to do this is with phototherapy, where the baby’s skin is exposed to a special blue light. The skin absorbs the light and changes the bilirubin to non-toxic forms, so that the body can more easily get rid of it in stool and urine.
The baby’s milk intake also needs to be increased. The process of removing waste from the body removes bilirubin in the baby’s blood. The milk also gives the baby’s liver the energy it needs to process the bilirubin.

In some cases, if the baby has very high bilirubin levels blood exchange transfusion may be needed. During an exchange transfusion, the infant’s blood is gradually removed and replaced with donor blood. This procedure removes bilirubin or lowers the bilirubin to safer, non-toxic levels.
In conclusion
The baby with jaundice has to be monitored and treated according to the severity of the disease. The baby can be fed breast milk and formula separately. Breast feeding is highly recommended but the mother should avoid foods that are rich in vitamin A, such as carrots, peaches, papaya, and sweet potatoes. However, these foods are essential for the baby’s growth. The doctor may recommend medications to reduce the level of bilirubin in the baby’s body.



